Shashank Tripathi’s research focuses on preventing and treating viral infections

As a kid on his way to primary school, Shashank would notice pigs frolicking in the mud, eating dirty leftovers, having the “best time of their lives” and yet staying healthy. He was intrigued. Why were they not falling sick?
His interest in the question grew after he had a severe case of food poisoning when he was in the fourth grade and was put on liquid diet for a month. He then started paying attention whenever others in his surroundings fell sick. What kind of disease did they have? Was it an infection or was it something that ran in the family? “These kinds of questions started very early with me,” he recalls.
Rather than medicine, however, Shashank turned his sights to research. After completing his Master’s degree in biotechnology, Shashank spent some time at Delhi University, trying to identify diagnostic markers for extrapulmonary tuberculosis (TB). Then, at the National Institute for Research in Reproductive and Child Health in Mumbai, he explored cardiac cell differentiation from human embryonic stem cells. In 2007, he started his PhD at the International Centre for Genetic Engineering and Biotechnology (ICGEB) in Delhi.
It was around this time that SARS-CoV was making headlines. It caught Shashank’s attention because mortality rates were as high as 30-40%. He joined Sunil Lal’s lab at ICGEB, which was working on SARS-CoV and other viruses. And it was here that Shashank stumbled upon the influenza virus. “The more I learned about influenza, the more I became fascinated about this virus, which to me, personally, is the most clever and amazing virus that we know of.” Four out of five pandemics in the last century have been caused by this virus, Shashank adds.
In 2019, after completing a postdoc at the Icahn School of Medicine at Mount Sinai, New York, Shashank joined the Department of Microbiology and Cell Biology at IISc as an assistant professor.
His lab at the Centre for Infectious Disease Research (CIDR) studies emerging and re-emerging viruses. “If you think about it, many findings that we have today related to molecular biology and biotechnology have resulted from studying viruses,” he explains.
Viruses usually produce a limited number of proteins due to their tiny genomes. However, they still have the ability to overpower their hosts, which can usually make tens of thousands of proteins. In addition, when faced with an antiviral hurdle, viruses can resist or escape it by rapidly changing their genome. This is why making vaccines against viruses is difficult. For example, in the case of influenza, often by the time a vaccine is produced and reaches the market, the virus has already evolved to escape.
During the COVID-19 pandemic, Shashank’s lab was one of the first in the country to set up cell culture and animal models for studying the effects of SARS-CoV-2. They also provided preclinical testing support to Gennova Biopharmaceuticals, the company that made the first mRNA vaccine in the country. Shashank says: “We were able to provide help to several academic labs as well as industries, not just in India, but globally.”
(Image: Sumandeep Kaur)
A major focus of Shashank’s lab is studying how infectious viruses penetrate host cells. This involves studying host receptors (cell surface proteins) that the virus contacts, host factors required for viral replication, and the host’s response to the virus – all of these can help develop more effective therapies and antivirals.
One such antiviral molecule that Shashank’s group has discovered is picolinic acid – a natural compound produced by mammalian cells – which can block virus entry into cells. This compound recognises the outer “jacket” or envelope made from components that the viruses usually steal from the first host cell they attack. Under normal circumstances, when infecting the next cell, the virus needs to shed this jacket, but picolinic acid does not allow the virus to take it off. “This molecule blocks the viral and cellular membrane fusion, thereby preventing the entry step,” Shashank explains.
Another aspect that his lab works on is repurposing existing drugs. His team spends a lot of time sifting through databases of approved drugs that can become potential antivirals. Out of the about 250 known pathogenic viruses, clinically approved antivirals exist against only eight, Shashank says. Even these antivirals are prone to becoming obsolete because the virus develops resistance via mutation. This happened in the case of a drug called Paxlovid used against coronaviruses, and Baloxavir for influenza – the latter took 40 years to develop but the virus was able to develop resistance within weeks of treatment. “You can spend years and years of research and billions of dollars … but the virus can quickly escape [from the drug] by acquiring a few mutations.”
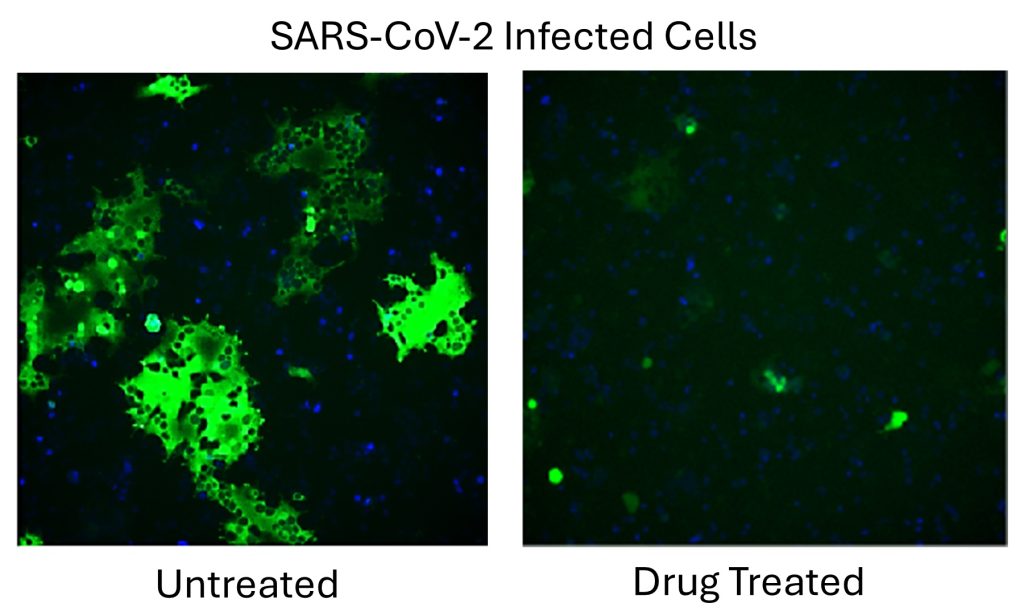
The solution, according to Shashank, is to target factors within the host cells, which virus desperately needs for its replication. Viruses can mutate their genome easily, but can’t do that to the host genome. This makes host-directed antivirals significantly less prone to viral resistance. Using such host-directed therapy in combination with antivirals can make them much more effective. Shashank’s lab has discovered that Auranofin – a drug approved in the 1980s for arthritis – when combined with Remdesivir is highly effective against SARS-CoV-2.
After SARS-CoV-2, the next virus that has the potential for a “red alert” situation is avian influenza, he says. While avian influenza initially infected birds, it has managed to cross the species barrier to infect seals, dolphins, and more recently, dairy cows in the USA. “What is worrisome is that the virus is getting more adept at infecting mammals,” he says. Shashank’s lab is currently trying to develop a “universal” influenza vaccine that can not only protect against circulating strains but also those that may mutate and emerge in the future.
Shashank’s lab also studies mosquito-borne viruses, with a specific focus on Aedes aegypti, a daytime mosquito, which hosts many flaviviruses like the Dengue virus, Zika virus, and Japanese encephalitis virus. “We wondered what is special about this mosquito. Why do all these viruses like this mosquito so much?” Shashank says. Answering this can help develop strategies that disrupt the insect’s ability to transmit viruses. His lab is also trying to pinpoint what human factors are preferred by these mosquito-borne viruses, which will help in developing broad-spectrum antivirals.
Yet another virus that Shashank’s lab is interested in is the one that causes the Kyasanur Forest Disease (KFD), which has been around for over 50 years, primarily in the Shimoga district of Karnataka, but has now spread across the Western Ghats. “It’s a neglected disease,” Shashank says, adding that there are no antivirals against the virus, and that the only available vaccineneeds to be updated.
“One thing I can say is that we are a very eager research group. We want to solve a lot of problems at the same time,” Shashank says.
What helps in this pursuit, he adds, is running his lab with the efficiency of an industry setup. For instance, the lab uses an in-house inventory system to track resources, and lab members are assigned responsibilities for maintaining instruments. Weekly research and literature meetings, weekly lab maintenance meetings led by students, focused group discussions, and daily one-on-one meetings with at least one lab member ensure research progress and smooth operations, he says. At the same time, emphasis is given to keeping the lab work environment relaxed via celebrating achievements, milestones and festivals; occasional group outings, and mandatory birthday celebrations of every lab member.

Shashank usually starts his morning by getting done with his emails and a few online meetings, then comes to the lab around 10 or 11 am. After picking up his son from school, he has lunch and then returns to the lab where he stays until 7.30 pm. He makes sure that he is available to his lab members for any professional or personal discussion at any time.
If not a scientist, what would Shashank have become? “A lawyer,” he says. “I come from a family of lawyers. I like this aspect where a lawyer would gather and present evidence to support their argument and prove a point. Science is also pretty much like that.”