Researchers are developing innovative tools to transport a variety of biological samples

(Photo courtesy: Deval Karia)
The COVID-19 pandemic has underscored the need for robust mechanisms to ensure rapid diagnostics and testing, especially for infectious diseases. Biological samples, such as swab samples collected for RT-PCR tests, need to be stored, maintained and transported to diagnostic centres quickly and safely. When it comes to the transportation of organs, which is crucial for saving the lives of patients with organ failure, the situation becomes more complicated. A major issue is that the infrastructure and transportation systems in Indian cities are not well equipped to handle the rapid and efficient movement of such organs. In this context, some researchers at IISc are working on different ways to improve these modes of transportation.
Biological samples are usually transported in fluid form via a cold chain in refrigerators or freezer boxes – a challenging prospect in remote locations. Blood samples can be transported in the dry state using blood spot cards, but these can carry only small volumes. The advantage of transporting samples in the dry state is that it doesn’t need a cold chain. This makes transportation of biological samples for diagnosing diseases like tuberculosis (TB) easier.
Caused by Mycobacterium tuberculosis (Mtb), TB is the number one cause of death by a single infectious agent worldwide , with a majority of deaths occurring in developing nations. Accurate diagnosis is key to controlling TB. An important step in this process is storing and transporting sputum – a type of mucus in the respiratory tract, coughed up during an infection – taken from patients. There have been only a few studies to transport sputum in dry form in the past in low volumes. It is necessary to collect a large amount of sputum from each patient to diagnose TB effectively, as the concentration of Mtb in the infected sputum can be very low.
To enable such transport, a team of researchers at IISc led by Bhushan Toley, Assistant Professor at the Department of Chemical Engineering, has recently designed a prototype device called specimen transportation tube (SPECTRA-tube). SPECTRA-tube consists of a cassette, comprising multiple layers of glass fibre membranes, in which the sputum sample is collected. Compared to conventionally used paper-based membranes – to which samples end up sticking – glass fibre membranes allow more efficient recovery of the sample in the end. The collected sample is dehydrated using desiccant packs that reside within the SPECTRA-tube. The SPECTRA-tube containing the sputum sample can then be transported to the testing facility, where it is reconstituted using a rehydration buffer. This technique has enabled almost complete recovery of the sample, an immense improvement over previous attempts, according to Bhushan.

“Because SPECTRA-tube allows a large volume of sample collection and transportation in the absence of a cold chain, this prototype can be distributed to rural areas for better diagnosis in low resource countries,” he explains.
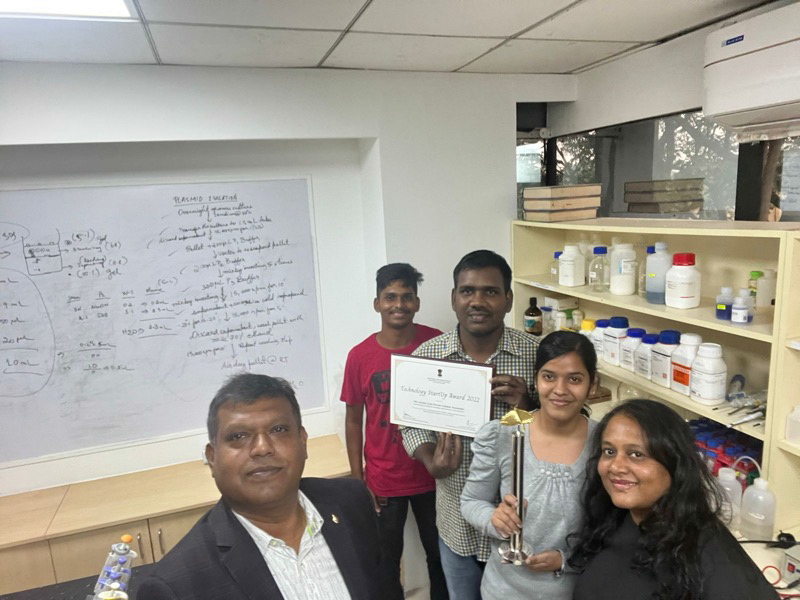
During the COVID-19 pandemic, there was an unprecedented increase in the transportation of biological samples – particularly RNA (ribonucleic acid), which is the genetic material of SARS-CoV-2. The RNA is usually collected and placed in a refrigerator for transport to the testing centre, but poor refrigeration or handling can damage the sample. Fathima J Benazir, co-founder and Chief Scientific Officer of IISc-incubated startup, Azooka Labs Pvt Ltd, and her team have created a solution called RNAWRAPR. Their device preserves the integrity of RNA and inactivates all substances that could affect its quality – such as enzymes or other biological molecules that can act on it – allowing its transportation without the requirement of a cold chain. “Samples remain stable at room temperature upto seven days after collection,” explains Fathima.
“Being in the field of molecular biology, we wanted to contribute towards the COVID-19 crisis. This led to the idea of creating a solution that can preserve the integrity of RNA samples and can be transported without any hassle and zero contamination,” she adds. “One of its greatest values is that it inactivates the virus in the media. Therefore, in cases of accidental spillage or exposure, it remains safe for the frontline health workers.”
Azooka is also working on extending the applications of RNAWRAPR to the transportation of other biological samples. “We have a series of products addressing sample collection for nucleic acid integrity across various sample specimens right from blood to biological fluids to tissues and so on, and also for specified applications like cell-free DNA. We are also working on targeting infectious disease sample collection, including TB,” Fathima adds.
While samples like RNA need smaller devices, moving entire organs is a much bigger challenge. They are currently transported via ice boxes and depend on civic authorities establishing green corridors (traffic-free routes) along the way. This has several drawbacks; it requires massive coordination between hospitals and several regulatory authorities and often, the time window is too narrow for the organ to reach the recipient. Deval Karia, a former MDes student at IISc, was inspired – after attending a course by faculty members B Gurumoorthy and Ashitava Ghosal at the Centre for Product Design and Manufacturing (CPDM), IISc – to develop LifeBox, a drone-based portable system that can extend the out-of-body time for the organ being transported. The project is currently led by B Gurumoorthy, Ashitava Ghosal and Manish Arora at CPDM, along with Dr K Balakrishnan at MGM Hospital.
The team decided to develop a system that would allow transportation of hearts for transplant surgeries. LifeBox uses a perfusion fluid and a patent-pending, novel refrigeration system. It is also equipped with multiple sensors that monitor the health of the heart, making it easier for the surgeon to make critical decisions. “A peristaltic pump drives the perfusion fluid from a reservoir to the heart which is housed within a chamber. Waste fluid from the heart is then collected. The heart in this setup is only intermittently perfused and does not beat,” explains Deval.
Currently, patients in need of a heart transplant spend long periods on waitlists for organs. For such patients, inventions like LifeBox could make a significant difference. Deval explains, “Factors such as debilitating illness, loss of employment, anxiety, isolation, and clinical costs take a severe toll on family members as well. Any method that reduces this waiting time will provide significant relief to all stakeholders within the system. Compared to aerial transport in chartered/commercial airplanes, this would significantly reduce costs for the recipient family too.”
Deval adds that they also plan on extending their novel refrigeration system to storing and transporting other organs, which may help in saving more lives.