Scientists at the Scripps Research Institute and the Evolutionary Venomics Lab (EVL) at the Centre for Ecological Sciences (CES), Indian Institute of Science (IISc) have developed a synthetic human antibody that can neutralise a potent neurotoxin produced by the Elapidae family of highly toxic snakes, which includes the cobra, king cobra, krait and black mamba.
The team adapted an approach used earlier to screen for antibodies against HIV and COVID-19 in order to synthesise the new venom-neutralising antibody. “This is the first time that this particular strategy is being applied to develop antibodies for snakebite treatment,” says Senji Laxme RR, PhD student at EVL, CES and co-first author of the study published in Science Translational Medicine.
The researchers say that this development takes us one step closer to a universal antibody solution that can offer broad protection against a variety of snake venoms.
Snakebites cause thousands of deaths every year, especially in India and sub-Saharan Africa. The current strategy for developing antivenoms involves injecting snake venom into equines like horses, ponies and mules, and collecting antibodies from their blood. But there are several problems.
“These animals get exposed to various bacteria and viruses during their lifetime,” explains Kartik Sunagar, Associate Professor at CES and joint corresponding author of the study. “As a result, antivenoms also include antibodies against microorganisms, which are therapeutically redundant. Research has shown that less than 10% of a vial of antivenom actually contains antibodies that are targeted towards snake venom toxins.”
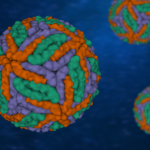
The antibody developed by the team targets a conserved region found in the core of a major toxin called the three-finger toxin (3FTx) in the elapid venom. Although different species of elapids produce different 3FTxs, a handful of regions in the protein are similar. The team zeroed in on one such conserved region – a disulphide core. They designed a large library of artificial antibodies from humans, which were displayed on yeast cell surfaces. They then tested the antibodies’ ability to bind to 3FTxs from various elapid snakes around the world. After repeated screening, they narrowed down their choices to one antibody that could bind strongly to various 3FTxs. Among the 149 variants of 3FTxs in public repositories, this antibody could bind to 99.
The researchers then tested their antibody in animal models. In one set of experiments, they pre-mixed the synthetic antibody with a toxic 3FTx produced by the Taiwanese banded krait, and injected it into mice. Mice given just the toxin died within four hours. But those given the toxin-antibody mix survived past the 24-hour observation window and looked completely healthy.
The team also tested their antibody against the whole venom of the monocled cobra from Eastern India and the black mamba from sub-Saharan Africa, and found similar results. The efficacy of the antibody was found to be nearly 15 times that of the conventional product. Crucially, when they first injected the venom and then gave the antibody after a time delay – 0 minutes, 10 minutes and 20 minutes – the antibody was still able to save mice. The conventional product, however, only worked well when injected alongside the venom. A delay of even 10 minutes significantly reduced the potency of the conventional antivenom.
In addition, the team used cryo-EM to tease out the crystal structure of the toxin-antibody complex, and found that their binding was very similar to the binding between the toxin and receptors found in muscles and nerve cells. “Our antibody seems to mimic the toxin-binding site of the receptor in our body,” says Sunagar. “Venom toxins, therefore, are binding to our antibody instead of the receptor. Since our antibody neutralises venom even with delayed administration, it may suggest that it can displace toxins that are bound to receptors.”
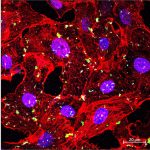
The researchers used human-derived cell lines to produce the antibody, bypassing the need to inject the venom first into animals like horses. “Because the antibody is fully human, we don’t expect any off-target or allergic responses,” Laxme adds.
“This solves two problems at the same time,” says Sunagar. “First, it is an entirely human antibody and, hence, side-effects, including fatal anaphylaxis, occasionally observed in patients being treated with conventional antivenom, can be prevented. Secondly, this would mean that animals need not be harmed in future to produce this life-saving antidote.”
The same approach can be used to develop antibodies against other snake venoms too, which can then be combined into a single antivenom therapy. On taking this forward to clinical trials, Sunagar says, “At this stage, a clinician cannot rely on this single antibody for treatment as this is only effective against certain elapid snakes. We are in the process of discovering additional antibodies against other snake venom toxin targets. A universal antivenom in future would consist of a couple of such synthetic antibodies that would hopefully neutralise venoms of most snakes in various parts of the world. A universal product, or at least a cocktail of antibodies that work pan-India, could then be taken to human clinical trials.”