Tuberculosis (TB), particularly in forms that affect body parts other than the lungs, can be tricky to diagnose. Researchers led by S Vijaya in the Department of Microbiology and Cell Biology have found a new, faster and more efficient way to use a host’s immune response to certain proteins unique to the bacilli to detect whether they have active TB.
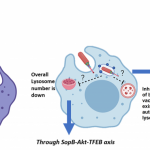
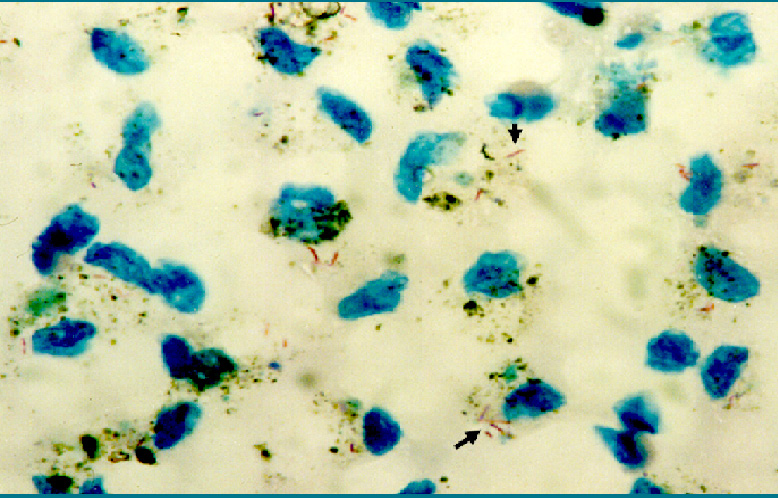
Immune cells in our blood have different sets of molecules on their surface – proteins, sugars, small compounds – depending on whether they are inactive as in healthy people, fighting a current infection, or remembering a past infection. The presence or absence of a certain unique combination of such molecules (called a biomarker) makes it possible to detect current disease in the body.
The team has discovered that active TB can be diagnosed if blood samples have immune cells with the following signature – having the biochemicals CD38 and CD4 but lacking CD27, while releasing a messenger molecule called Tumor Necrotic Factor (TNF-α). They added TB antigens to a blood sample to trigger an immune reaction.
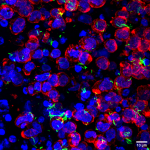
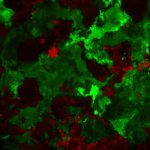
By analysing the presence or absence of marker proteins on T cells in the sample using flow cytometry, they were able to accurately diagnose TB.