Rachit Agarwal’s lab focuses on engineering treatments for TB and osteoarthritis

Rachit Agarwal’s tryst with bioengineering was always destined. Born into a family of doctors, including his father and elder brother, he was exposed to medicine from early on. School nurtured his interest in biotechnology. “I was naturally interested in science simply because I was good in those subjects. I liked maths and physics quite a lot. Then I got interested in biotechnology, because there was a lot of buzz around it while I was in higher secondary school,” he recalls. “That prompted me to opt for biotechnology as my undergraduate degree from IIT Kharagpur.” During his undergraduate years, he dived into different fields, including biomedical engineering.
Rachit then decided to pursue a PhD at the University of Texas at Austin in Krishnendu Roy’s lab, where he worked on the delivery of cancer drugs using polymeric carriers, studying whether the latter’s shape has any effect on the delivery. He found that manufacturing non-spherical particles was quite difficult, and so he collaborated with a semiconductor manufacturer to print the required shapes. “We adapted the way they printed transistors … and started printing our polymeric particle.”
Rachit went on to do his postdoc at Georgia Tech with Andrés J García, and became inspired by his style of leading the lab and mentoring people. “In Andrés’ lab, I was given a lot of freedom, and I worked on multiple projects. My PhD was a bit niched because very few people were working on anything similar, but my postdoc helped me expand my knowledge and expertise in varied techniques and projects,” Rachit recalls. His work there revolved around bone tissue engineering and designing inhalable carriers to treat lung infections.
After his postdoc, Rachit moved back to India. “I wanted to come back to India for several reasons. When I went [to the USA], I always felt that I would come back; my family’s here. I also felt at the time I was doing the postdoc that research in the USA is getting quite saturated, in terms of funding and freedom as to what you can work on,” he says. The transition brought some challenges like added administrative responsibilities and delays in procuring lab equipment. “You suddenly get an idea, and you want to work on it as quickly as possible, but then you have to wait for 2-3 months before you can actually start working on it, because that reagent you need is not available and it takes time to come in.” But things have been improving, and people at IISc are helpful and remain open for collaborations and discussions, he says.
Rachit’s lab at the Department of Bioengineering currently targets two major healthcare challenges: tuberculosis (TB) and osteoarthritis.
His team is trying to develop drug delivery methods for TB that are more targeted and less toxic. In India, many patients tend to discontinue the treatment, either because they can’t afford it or because of side effects that accompany the current oral administration of antibiotics. Rachit’s lab is keen on using approaches which are more patient-compliant, shorten the treatment duration and reduce side effects.
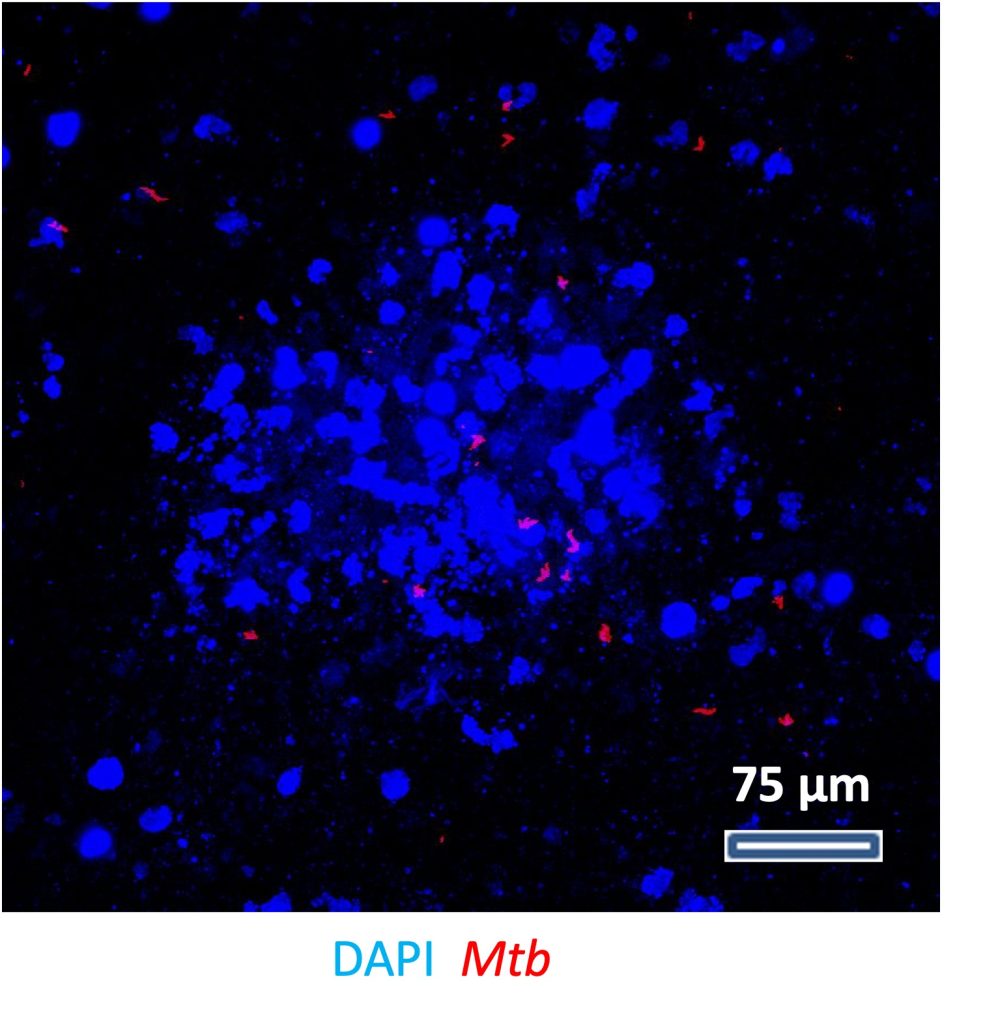
His team is also developing 3D models of human tissues to understand TB biology better. There is a major gap in this area because TB develops very differently in humans compared to conventional animal models. Mtb (Mycobacterium tuberculosis), the causal organism, is an obligate human pathogen – it depends on the human host to survive – and thus does not infect other mammals like mice in nature. Mice also do not show latent TB, which is quite common among humans. “The idea was: Can we use materials and human components and recreate the human environment … then there will be a very powerful tool to examine what can harm the bacteria, what drugs would work, and so on.”
The 3D models his lab is working on can help scientists understand the environment of TB granuloma – small nodes of bacteria formed in TB – and develop better treatments.
In a recent study, they found that a 3D model they have developed behaved much more like actual human tissue compared to the 2D cultures currently used. The model uses collagen – a common protein found in the extracellular matrix of the lung – and has matching mechanical properties like lung pore size. It shows better outcomes in gene expression, cell behaviour and response to infection when compared with 2D cultures, the team found.
“There’s a drug called pyrazinamide for TB treatment, which is widely used in clinics. It was discovered back in the 1970s and was directly tested on mouse models. What is still a mystery is that if you test it in 2D culture, it does not work at clinical concentrations, and you must use 8-10 times the concentration to see any effect,” Rachit explains. “However, in our model, we found that pyrazinamide still works at the clinically relevant concentration, and even at lower concentrations. This is a validation that our model is more representative and can be used for drug discovery more efficiently than 2D ones.”
Apart from TB, Rachit and his students are also trying to develop vehicles that can carry drugs to the joints of patients with osteoarthritis – a degenerative disease causing pain and stiffness – to halt or reverse its progression. Current treatments are limited because either they are given orally and work like painkillers that temporarily relieve the symptoms, or they are given as injections directly to the patients’ joints, but only by trained personnel. Instead, Rachit’s team decided to formulate an injectable polymeric carrier that can release the drug slowly in a sustained manner over extended periods of time, thus reducing the frequency of such injections.
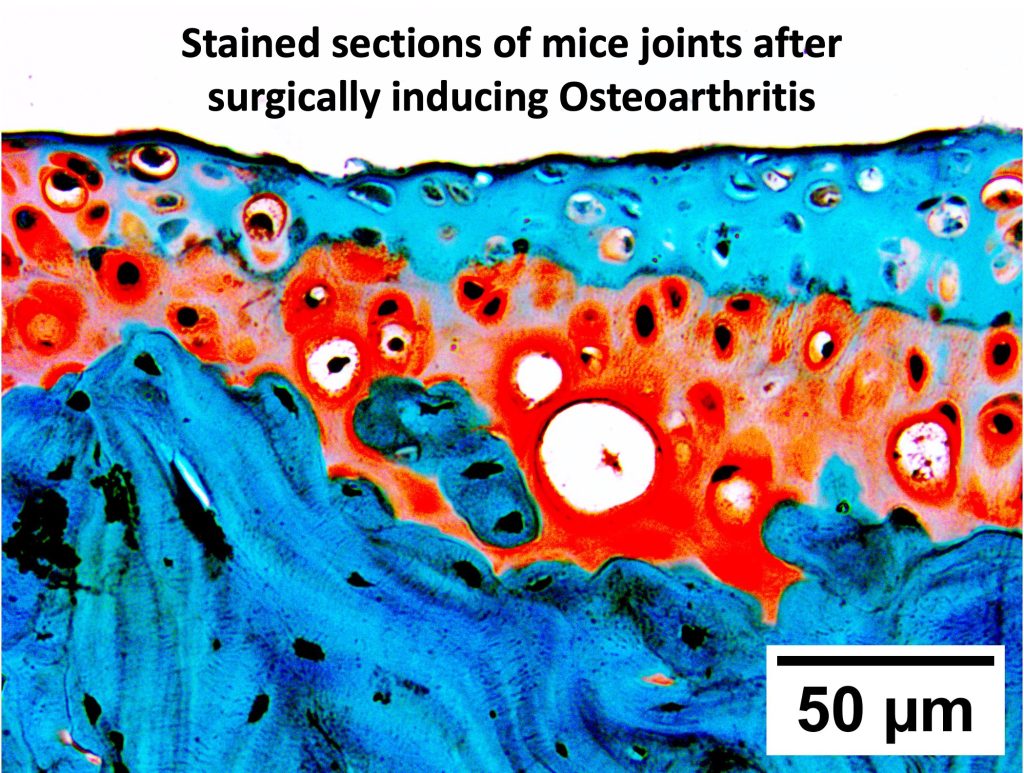
Rapamycin is a drug that induces autophagy – clearance of dead or damaged cells – and is used to treat many conditions. In a recent paper, Rachit’s team showed that rapamycin is more effective in treating osteoarthritis when delivered using their polymeric particles. “If you give one or two injections of the free drug at these concentrations in the animal [model], it continues to develop osteoarthritis. Whereas, if we use our particles, it completely stops it. Basically, osteoarthritis did not develop over a period of the 2-3 months that we tested,” Rachit explains.
In the coming years, Rachit is keen on taking forward his research to the clinic. His long-term goals include developing a potential TB vaccine and inhalable delivery of TB drugs. On the osteoarthritis front, they are also seeking to reverse disease progression. “Most [osteoarthritis] patients come to the clinic after they have accumulated severe damage in their joints. So, we’re looking at the introduction of growth factors and other things that can help repair the damage that has already accumulated in the tissue.”
Apart from doing research, Rachit likes to play snooker at the faculty club. Tennis and trekking around Bangalore are other hobbies he takes time out for on weekends. “At the moment, I have two small kids and so, all of these hobbies have come down, and these kids have taken over most of my time. I’m looking forward to them growing up and joining me in these activities,” he adds.
The fact that the diseases his lab is studying have such high rates of prevalence, morbidity and mortality is what keeps him motivated to do research every day, he explains. “The other motivation is to understand things that we don’t understand. That’s the whole reason I went into science and eventually PhD. That still drives me.”